Trauma Update - Adding Some Clarity
I have recently returned from a trauma conference in the UK where amongst the topics we discussed was the very hot issues of self-extrication, the use of cervical collars and spinal boards during extrication and onward transport of the patient.
It is clear to me that the opinions published online (and particularly on social media) are leading to some confusion amongst fire fighters and rescuers around the world who regularly perform this kind of rescue operation.
Firstly and most importantly, you simply MUST stick to your local operating policy and procedures; you cannot and should not deviate from them. Reading the latest evidence and agreeing with it is not licence to operate in a way that is not promoted by your emergency service agency. I appreciate that this is frustrating and I already talk to people who find themselves unable to deliver what theyconsider to be the best patient care due to (what they perceive to be outdated) local policy.
So where exactly are we; what is the latest thinking from a medical perspective? Well let’s look at it carefully.
Self-Extrication – Really?
Following a collision the occupant of a vehicle may be able to extricate themselves. Asking a person if they can stand and get out of the car is nothing new and indeed I have taught this concept for a number of years as a first consideration. A recent study has shown that more forces may be applied to a patient if they are extricated in a conventional way versus them self-extricating. Opinion is divided on this study for several reasons; primarily because it is (at this point) just a single study and more research is needed. However, the conclusion certainly is food for thought. We need to understand that the human body can (in many circumstances) provide its own best mechanism for self-preservation and an alert patient will develop a position of comfort with muscle spasm therefore protecting a damaged spine. Recent research also indicates that as little as 2% of vehicle occupants are found to have a spinal injury after a road traffic collision. Please remember that despite the latest evidence and research, every extrication and each patient must be carefully assessed to ensure the right plan is being implemented; self-extrication should only be a consideration and not a mandatory plan of attack, and only carried out with medical support.
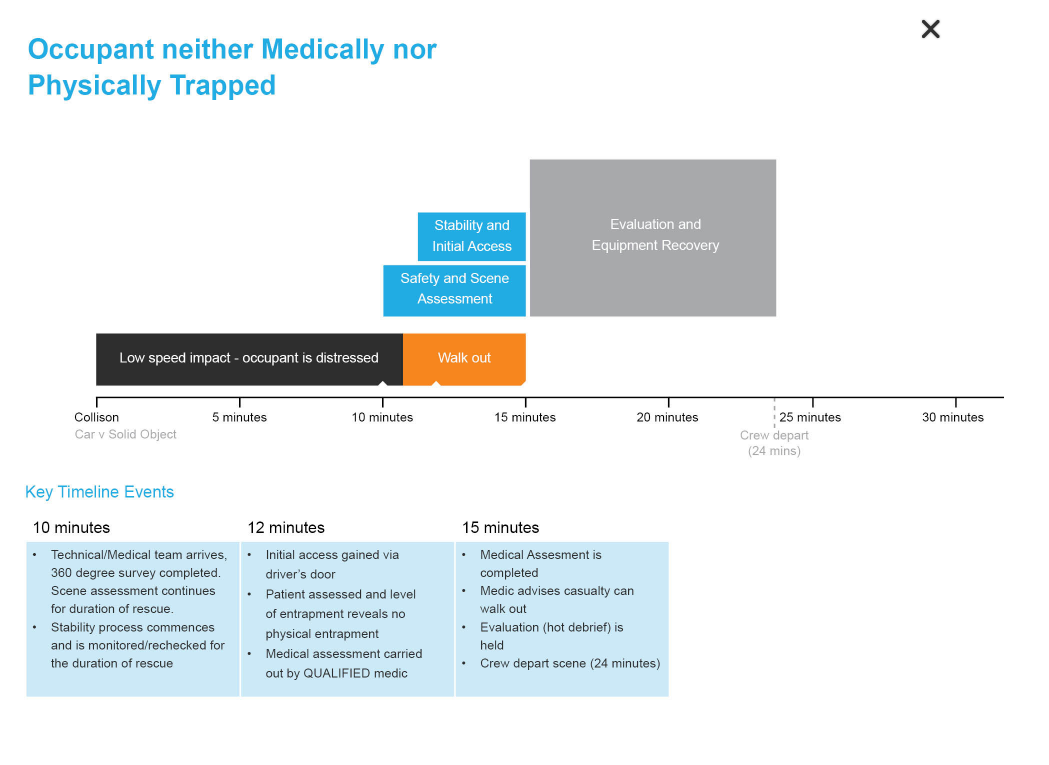
This is is what the timeline in case of a self-extrication will look like:
Collars and Spinal Boards
We have always been taught the importance of spinal immobilisation and in order to help us achieve this we have (where possible) generally applied a cervical collar at the most appropriate time. The evidence to support collars is scarce and contradictory evidence is emerging of the negative effects they can bring. A consensus statement written in 2013 is still valid. At the conference I attended several speakers recommending not to think about “spinal immobilisation” but rather focus on “spinal care”. Immobilisation is not harmless and the methods we use (KEDs/Collars/Boards) tend to stay in place until the patient is far along the care path. In other words: collars can (and often do) stay on needlessly for much longer than is necessary (well into the patient's stay in hospital). Collars can increase intracranial pressure; manual inline stabilisation does not.

Is this really the end for the humble collar? The evidence would suggest it is!
Whilst spinal boards are excellent for extricating a patient there is a definite shift away from using them as a transport device. The popular method now is to ‘scoop’ the patient from a spinal board (using a scoop stretcher) and place them either on an ambulance trolley (as in Queensland, Australia) or on a vacuum mattress. A vacuum mattress will provide much more ‘sympathetic’ support as opposed to a rigid board which is very uncomfortable.

Has our "Full Immobilisation" approach been innapropriate? Too much?
Conclusion
I have often said that the medical aspects of rescue change far more quickly than the technical aspects. This can leave individuals and organisations frustrated at the rate of change and technical rescuers (fire & rescue services) find it difficult to keep up, principally because of the need to retrain their staff.
The purpose of this blog is to try and add some clarity not to what you necessarily do, but to explain the current thinking and how you can incorporate this in your future discussions and professional development. Also in some parts of the world, you may have a medic on scene who can incorporate this latest thinking, so you may be expected to figure this into your plan.
I accept that my attempt to add some clarity may have muddied some waters, but things are changing and we have to keep up!
As ever, I welcome your feedback.
Ian Dunbar